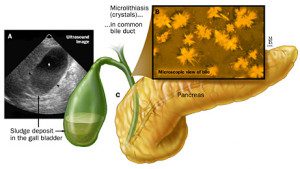
 Biliary Microlithiasis, sometimes referred to as gallbladder sludge, is made up of cholesterol monohydrate, calcium bilirubinate, or calcium carbonate stones measuring less than 2 mm. Sludge is a suspension of crystals, mucin, glycoproteins, and cellular debris.
Biliary Microlithiasis, sometimes referred to as gallbladder sludge, is made up of cholesterol monohydrate, calcium bilirubinate, or calcium carbonate stones measuring less than 2 mm. Sludge is a suspension of crystals, mucin, glycoproteins, and cellular debris.
Have you been diagnosed with Idiopathic Acute Pancreatitis?
You have?
Well that means your doctor has no clue or concrete evidence explaining WHY you have had acute pancreatitis or recurrent acute pancreatitis. Chances are your pancreatitis isn’t idiopathic at all. Up to 79% of idiopathic pancreatitis cases can be traced to biliary microlithiasis.
Biliary Microlithiasis On Endoscopic Ultrasound
The following video will show you EUS pictures of biliary microlithiasis along with some other causes of acute pancreatitis. It’s slow moving but I found it interesting. You may find it to be as exciting as watching the grass grow on a hot day but watch it anyway. You may learn something you can share with your doctor. But be advised most doctors don’t seem to like patients who may have more knowledge than themselves. 🙂
Biliary Microlithiasis Leads To Pancreatitis
 Biliary Microlithiasis may lead to pancreatitis through several mechanisms. Small stones may transiently impact the papilla, leading to pancreatic duct obstruction and eventual pancreatitis. Repeated exposure to microlithiasis may lead to papillary stenosis and SOD, both of which are associated with pancreatitis.
Biliary Microlithiasis may lead to pancreatitis through several mechanisms. Small stones may transiently impact the papilla, leading to pancreatic duct obstruction and eventual pancreatitis. Repeated exposure to microlithiasis may lead to papillary stenosis and SOD, both of which are associated with pancreatitis.
Like gallstones, sludge may cause obstruction. Gallstone pancreatitis is usually related to small stones, which may not be detected by conventional cholecystographic techniques. So …
The question you should be asking your doctor is: Is my pancreatitis really idiopathic or is it really a form of gallstone pancreatitis due to biliary microlithiasis?
Interesting, but how does one treat biliary microlithiasis? That is the million dollar question.
Hi Peter – “how does one treat biliary microlithiasis?” you are right “that is the million dollar question.” Those who promote gallbladder flushes would tell you that is how to rid yourself of the small stones and “sludge.” But that sounds really risky to me simply because epson salts can be toxic in large doses and the amount of olive oil would certainly cause an acute pancreatitis attack in those who already have a damaged pancreas. The other potential problem I can envision is that the stones and or “sludge” get hung up in the bile duct or pancreatic duct and actually causes gallstone pancreatitis. So I certainly don’t think this is a safe alternative but that’s just me. I could be wrong.
My idiopathic acute pancreatitis attack was May 30, 2014. The hospitalists decided that the cause of the attack was due to excessive use of ibuprofen. My PCP did not agree with them. I spent most of the summer recovering, but food caused me some kind of discomfort, most of the time. So, I went back to my PCP and he passed me on to a GI and Liver Specialist. I had blood work, ultrasound of the gall bladder, and MRI of the pancreas (MRCP?). The MRI showed my pancreas looking normal. The ultrasound of the gall bladder showed a “small amount” of sludge. The doc didn’t define”small.” His recommendation, based upon the fact that”pancreatitis can kill you,” is to have my gall bladder removed. At first I just took his recommendation in a matter of fact kind of way. Now, I am balking. I have had one invasive surgery in my life and it caused complications. Do I really want another one? I have heard that after gall bladder removal there can still be some bad complications and that you end up eating low-fat anyway. I need more information. For sure, I don’t want another attack of acute pancreatitis. Who knows about the the gall bladder removal treatment, and what can you tell me?
Hi Jody – gallbladder sludge also called microlithiasis can and does cause acute pancreatitis. All surgical procedures carry risk. Gallbladder surgery is no exception and some people even die from it, especially older patients who need emergency gallbladder surgery for some reason like acute cholecystitis. Passing gallstones can be uncomfortable, some say horrible, but the real worry is 1) acute pancreatitis that can kill you or make you wish your were dead because you have so much damage, 2) acute cholecystitis which can also become life threatening and 3) SOD which can occur due to scarring caused by gallstones passing. SOD also commonly causes acute pancreatitis. With this information in mind you still need to make your own choice as to whether you have your GB removed or take your chances. There are several videos on this post about gallstone pancreatitis that may help you with info as well. Good luck to you 🙂
Hi Jody,
Did you decide to have your gallbladder removed or not? I also have to make the decision soon. Would appreciate your experience. thanks.
Ferdinand
Ferdinand she may not be active. People come and go because it is an info site not a forum. I should think about adding a forum.
I am still here. I was asked earlier how the gallbladder sludge was diagnosed. It was an abdominal ultrasound. The first GI specialist said my gallbladder needed to come out. Eventually, I sought a second opinion and that doctor said, “90% of us would tell you to have it taken out, BUT, that doesn’t guarantee you won’t get pancreatitis again.” That really eased my concerns! I finally made an apointment with the surgeon earlier this year. He decided to order another ultrasound. So, I fasted for 8 hours and went to have the ultrasound. That night they told me my gallbladder was “unremarkable.” I was told by the GI docs that sludge was sludge and the amount did not matter. They also made me think it would not go away, but the second ultrasound seemed to show something different. That is not to say that I don’t sometimes have discomfort, a little bit of pain now and again, and a few times have felt bad enough to go to bed. Health guy is right about fat. I have used is protocol to abate an impending attack more than once. Some of us take longer to learn.
I read your article on Gall Blader sludge and it’s relation to Idiopathic Acute Pancreatitis. Perhaps that was the root cause, but I still have my Gallbladder and they have never felt the need to remove it.
The low fat/low protein recommendation was on the Natl Pancreas Foundation site. They indicated fat and protein could both stimulate the pancreas. Is cholesterol just another form of fat? Mine is good now after all the weight loss. Do I need to be concerned about it like fats? TY Rob
Rob, yep cholesterol and triglycerides are actually molecules called lipids. THAT is an over simplification because lipids contain more than fat but high blood fat levels can and do cause acute pancreatitis. I’m not talking about cholesterol or tris that are around a couple hundred. It takes levels in the thousands to become a pancreas problem. So if your cholesterol is a little high you may have an increased risk for clogged arteries but not pancreatitis. “Mine is good now after all the weight loss.” SEE! Good things come from everything 🙂
I have had 11 pancreatitis attacks since June 15th. We thought the first one was food poisoning. They are horrible! I have been to the hospital 4 times with this and some I try to ride some of them out at home. My husband travels so I am alone and cannot move, these get so violent and debilitating. When it gets to the peak I faint, and on one I knocked my 2 front teeth out while fainting. No doctor will commit that it is acute pancreatitis, some say viral gastritis. After all my reading, it really sounds like IAP. The doctor who did my upper GI said I did not need to do an endoscopic ultrasound, the regular ultrasound turned nothing up, nor did the CT’s, though my amylase and lipase are high but not as high as some people, but we are all different so since it is higher than normal, it seems to be enough to throw me into these violent attacks. I am seeing a Naturopath now because he is the only one who will listen to me. I do not drink, nor am diabetic, but still a sugar junkie. I also gulp my food so since there are so few enzymes getting to my food, I think it just sits in my stomach, not digesting but fermenting and putting off AH, the toxin that alcohol does, since it is fermented sugar too! I am at my wits end. I cannot keep going through these attacks! What does one have to do to get an endoscopic ultrasound to rule out Biliary Microlithiasis?
Hi Laura – sorry to hear you are ill and having a rough time. The old regular ultra sound is the best single test for finding gallstones and sludge. It will also show panc damage. CT is very good for diagnoosing pancreatitis (72 hours or more after onset) and damage however EUS is more sensitive for finding chronic pancreatitis, especially what is called minimal change CP. EUS and MRCP may also be beneficial in finding stones lodged in ducts. How high was your lipase (most specific for pancreatitis) and amylase? Sometimes you just need to keep on the doctors. Hang in there. I’m not sure a naturopath will be that much help in diagnosing your condition because to my knowledge they can’t order medical tests unless something has changed in the rules regarding their profession.
Hi Laura, has your situation improved?