 Questions I see often within comments on my site are “Do I have pancreatitis” or “Could I have pancreatitis” or “Do you think I have pancreatitis?”
Questions I see often within comments on my site are “Do I have pancreatitis” or “Could I have pancreatitis” or “Do you think I have pancreatitis?”
Unfortunately I was too lazy (among other reasons) to invest 8 – 12 years in school and residency in order to become a doctor so …
I can’t diagnose anyone who visits and or comments on this site.
I also can’t prescribe a course of treatment. And …
These facts are pointed out in various places on this site including the terms of service page. But …
What I can do is point out my personal experiences and pass on the information I have learned from other sources (articles written by doctors and scholars) thereby giving you the information that may help you to determine a course of action.
One thing I need to point out which is this:
Pancreatitis can kill you. So …
 IF you have any symptoms that would trigger immediate concern, even fear in a prudent person …
IF you have any symptoms that would trigger immediate concern, even fear in a prudent person …
GO TO THE NEAREST ER!
DO NOT try to diagnose yourself.
Do NOT look for more information on the Internet.
Go to the nearest ER if you even suspect acute pancreatitis because …
In the case of pancreatitis, like other deadly conditions, it is ALWAYS better to be looked upon as a LIVE hypochondriac rather than a dead or maimed (disabled) victim who did not seek proper medical care in time.
What IS Pancreatitis?
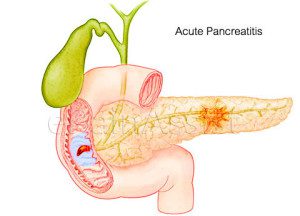 Simply put pancreatitis is inflammation of the pancreas. There are two (2) main classifications of pancreatitis.
Simply put pancreatitis is inflammation of the pancreas. There are two (2) main classifications of pancreatitis.
Acute and chronic.
The acute condition appears or happens rapidly. You can be or seem fine one minute then become sicker than a dog the next.
The pancreas becomes inflamed due to various circumstances.
This inflammation can result in prematurely activated pancreatic enzymes becoming trapped within the pancreas and digesting the pancreas which causes damage.
Pancreatitis can become life-threatening very quickly. This is why you should go to the nearest ER if you suspect that you could have acute pancreatitis. It’s nothing to fool around with. Go to the ER.
What Are The Normal Classic Symptoms?
 There are classic symptoms for all diseases and conditions but that doesn’t mean those diseases and conditions always play by the rules or go according to the known knowledge of the day. Symptoms can vary but for the most part acute pancreatitis presents like this:
There are classic symptoms for all diseases and conditions but that doesn’t mean those diseases and conditions always play by the rules or go according to the known knowledge of the day. Symptoms can vary but for the most part acute pancreatitis presents like this:
Pain – The pain comes on fast like a freight train, without brakes, going down hill. It can be so intense it is difficult to breathe, difficult to sit still (you may rock back and forth). You may find yourself leaning forward instinctively to help ease the pain. The pain is steady, constant. It does not come and go. It often radiates to the back behind the rib cage. Not behind your shoulder, behind your ribcage. The pain will most likely be the most horrific you have ever experienced.
Nausea and Vomiting – You may have nausea and vomiting and you may not. Sometimes the nausea and vomiting can be severe, relentless. In other words you may puke your guts up, continuously. Vomiting does not relieve the pain.
Other symptoms may include:
- pain is usually worse lying down
- swollen, tender abdomen
- chills
- cold sweats
- fever
- rapid pulse
- rapid and/or difficulty breathing
Complications that may arise in severe cases include:
- infection
- necrosis
- hemorrhage
- shock
- organ failure
- death

Alien not pancreatitis
It is interesting to note that acute pancreatitis does NOT always present with “classic” symptoms.
I’ve read case studies where there was no pain (RARE) however, the patient had severe vomiting.
I’ve read comments from people who have experienced very little pain (again rare) and were surprised to find out they had pancreatitis. So …
It is entirely possible to have the condition without the classic symptom of severe pain.
NOTHING is 100% indicative.
That is why it is important to get a complete work up at the ER where they can use a battery of tests to determine whether you have pancreatitis.
If you have any of the classic symptoms or any of the secondary symptoms or a combination of classic and secondary go to the ER and get worked up. Find out what is wrong.
Finally, I found a site with information that gives me hope!! I was diagnosed with Cambridge V Chronic Pancreatitis due to pancreas divisium. I’m so angry that it took 49 years for a physician who cared enough to order a CT scan to find pancreatitis. I had a cardiac arrest at 28 years old, respiratory failure twice and kidney failure. They did two heart ablations, heart meds and due to experimental tubes they used through my femeral artery for a heart pump when I arrested I’ve had two femoral artery bypass surgeries because a clot formed due to artery damage when they took it out. So I have literally been through hell since then.
After seeing a gastroenterology doctor and having a MRI and a ERCP in which they placed two stents in to open the bile ducts, they said my pancreas has calcified and irreversibly damaged.
Upon a second E Yet CP the surgeon said he took the stents out and I didn’t need any more placed at this time. I thought ” hurray, there’s hope”. Then I received a dictation of the procedure and in it the surgeon diagnosed Cambridge V chronic pancreatitis due to pancreas divisium. And as I read this outline of how bad my pancreas is damaged, it says that upon looking for the stents that they were not visible and had dislodge and unretreavable. It’s been two weeks and they sent me to a pain management doctor who wants to do an injection through my back to hit the pancreas nerve to numb it for up to 8 hrs. Gave me Percocet and neurontin. They asked me about anxiety, stress and depression, I answered truthfully about feeling overwhelmed and feeling doomed. Hell the doctor said I was doomed so I believed it right!! Well now they say I have to talk to a psychologist so that they can be sure I won’t treat my anxiety with pain meds. WTH!
So I have been up now in a attack for 48 hrs. I am sure that it’s been triggered by the new meds and, or the stents the surgeon left in me has caused it!?? Idk and I called and called the doctors office with my concerns and no return call yet.
I am lost , and so confused about what I need to do to stay alive, and these attacks hit and I suffer for days on end and wonder how I am going to be able to live with this condition. It’s too much!!
I read your advise and how you feel about the medical profession when it comes to the way they treat this, and I felt that I have hope after all! I’ve started the ibuprofen today and just praying it kicks this inflammation fast.
Thank you and god bless you for taking the time to share your story. Darla Burbank
Hi Darla – You’re welcome. I am truly sorry you have to go through the horrors and agony. I wish I knew more about pancreas divisum but I don’t. I know a little but a little information is sometimes dangerous. I think diet, supplements and Ibuprofen my help but they will NOT cure you. I don’t want to give you false hope but I don’t want to dscourage you either. I think pancreas divisum definitely makes this “crap shoot” called pancreatitis more difficult. Let us know how things go. 🙂
Dear Healthy Guy, I discovered your blog few weeks ago after running around YouTube for any answer what might be going on. Reading it makes me enormously grateful for taking the time and effort keeping all updated. Thank you.
Some advise, please.
I think I am somewhere in a beginning of it.
December 2019 I was in a hospital with depression and there they took blood that showed elevated level of enzymes indicating issues with pancreas. What exactly, lipase or amylase, not sure. 87 first result after eating, 75 next morning before breakfast. Asked, do I have any pain, nausea, but no, all not included. Was said not to worry.
Mid January suddenly felt dizzy and nauseous, heading to toilet thinking something will come out, but nothing. Heavy tiredness and with an hour it was gone. Next day slight dizziness and nausea. It started to send me all week, with slight uncomfortable feeling (throbbing) in the stomach.
I went to see a doctor, they took blood, the level of lipase was 84. Again, should not worry. Despite of that I decided to go very simple food list. Oat, rice, steamed veggies. With one week the discomfort was gone. Lasted two weeks until I made salmon with butter. Three hours later the feeling of nausea returned with increasing very mild pain. It continued days after, so I took my steps to a doctor again who took blood that showed all normal. Ultrasound found anything wrong.
Nothing to worry about. But I did and do.
I went back while no change there. They took blood again. I had a call yesterday evening from a doctor saying level of lipase has risen to 120.
The first night now I woke up slight pain in my abdomen, it seemed not to be at one spot. Left side is pain free, right side is troublesome. And around belly. No pain radiating back, no vomiting. No fever.
Asking from the doctor does it all indicate a acute (but very mild form of it) pancreatitis the answer was no.
Might I already developing a form of chronic pancreatitis?
Asking this from you is not the best idea, you have said , but as you have read so many stories, went through turmoil yourself and digested piles of research I humbly through the question above where could it all lead?
No alcohol, no cigarets and been relatively healthy eater.
Regards, risto
Risto – sorry to hear you are feeling ill and don’t know why. Yes, it does sound like you may be in the beginning stages of pancreatitis. It could be either form AP or CP. Has anyone in your immediate family had similar issues? If so was it diagnosed? And what was it supposedly? Did it improve, go away or continue and get worse? Have you considered genetic testing for gene mutations? You may have a genetic variant that predisposes you to pancreatitis. Do you have any autoimmune diseases that could be causing havoc with your pancreas? Do you take medications for conditions and those meds maybe be the culprit?
Hi, thank you for your reply.
I have asked my family and no one has ever had any issues with pancreas.
I went to ER the other day while my family doctor couldn’t help me on. They took huge amount of blood, made new ultrasound and I waited the results. Lipase was 107, ultrasound showed no abnormalities with pancreas. I was given a paper with all the results that said chronic gastritis. No explanation why the level is elevated though. How to continue…Appointment to endoscopy is in July.
I would say it is getting more difficult to figure out what can I eat or how to behave in a long run now. Knowing that the symptoms can mimic themselves (pancreatitis and gastritis) it leaves me hanging cold.
It is so not cool to admit that the discomfort has increased. Feels extremely lonely right now.
I have been wondering about the case around autoimmune abnormalities, but somehow any of the doctors I have visited have not suggested finding it important to search the cause there.
Anybody at this point do not think my pancreas is giving me a trouble.
Kind regards,
Risto
Risto – do not become discouraged. It often takes several attempts for doctors to actually get a right diagnosis. The fact that fat seems to cause problems seems indicative of a pancreas, gallbladder, liver or sphincter of oddi problem. All of which are often or always irritated by fat consumption. Celiac disease can also cause what I call minor pain but often severe nausea, vomiting and diarrhea. Celiacs often have elevated lipase levels (not sky high just elevated like yours). Get tested for Celiac disease (blood work will rule it in or out). It could also be an H. Pylori infection (again blood work) or gastritis as mentioned as a diagnosis. Good luck. I hope you feel better soon.
Wow Darla . You’ve been through hell . I’m so sorry this has happened to you , I’m going through this rt now and it sucks I can’t believe how painful this is …. I wish you well feel better kick ass girl. Love Deb wegmann
Hello, I am one of those people who has never had pain to indicate pancreatitis. I was an extremely healthy woman age 51 when I unwittingly ingested a bacteria that immediately made me nauseous. I went to the doctor two weeks later and was met with a blank stare. I went home with not as much as a blood test. The nausea slowly increased over the last four and a half years. There was a point in time it went away for several months with the aid of very strong lemon with a bit of water several times a day. The doctor told me to stop drinking it because it would damage the stomach lining. The nausea came back soon after I stopped.
I thought the nausea must be from the bacteria but it took 4.5 years to get a doctor to prescribe the only antibiotic that works on the upper GI, which I had to pay for out of pocket, $1700, because no one would refer me to a Gastroenterologist. Gastroenterologists are the only doctors that are approved to order it. The antibiotic Xifaxan combined with Emycyn, gave me my energy back with in a few days, but the pancreas did not improve. I went to a new doctor who gave me who finally ordered Lipase test which indicated Chronic Pancreatitis. He then referred me to a Gastroenterologist. I have zero problems with my bowels since taking the Xifaxan.
The Gastro doc performed all the usual tests, ct scan, endoscopy, ultrasound etc…but I have to wait six months to get in to see him and discuss his findings. 1.5 months to go.
I just wanted to tell my story for those who have no pain. Perhaps they will know to demand a Lypase test before it’s too late. I had 4.5 years to damage my pancreous, where I had the opportunity to find out within two weeks if the doctor had treated me with the least bit of respect. Only a few months ago I went to Italy and had a glass of wine and Gelato with dinner for ten days. This was very unusual for me because I’ve never been much of a drinker. Sadly this trip turned my morning nausea into an everyday constant nausea.
I’m grateful for your site and the information you have shared. It’s so very kind of you to take the time. I have started following a diet using the foods you recommend and I’m feeling better much better. I truly Thank you! – Joni
Hi JJ – It is unusually rare (but not non-existent) to only have nausea and no pain. MY CP produces mostly nausea (when I over step bounds) but the acute phase is a whole different story. Glad to hear the diet helped. Sorry you had to suffer for almost 5 years needlessly. Someone should have done better by you. Hopefully you’ll get a handle on your CP and keep it tightly controlled. By the way grape seed extract works very well to help control nausea, reduces, even eliminates the inflammation in proper doses.
Hello Healthy Guy, I’m another reader convinced that you are Heaven sent! ?
Vomiting, diarrhea & servere abdominal pains landed me in the ER and diagnosed as having a pancreatitis attack, UTI & the flu. For 3 days I was on bowel rest, given antibiotic & pain meds interveniously then released advised to eat a low fat diet & take Pantoprazole Sodium. One week later, because of abdominal pains & nausea returned, I ended up back in ER but lab test said it wasn’t another pancreatitis attack. Now months later, I have off & on center area radiating abdominal pain & lower right side of my stomach is tender. I’m gassy & belch after meals. It’s apparent something is going on with my digestive system. (going to fast & start a food journal as you suggested). Dr said 2nd ER visit seems like IBS but GI dr said it wasn’t. Test ruled out the gallbladder or any stones. I’m an occasional drinker but haven’t had a cocktail since my bday in January & this all began in March. What additional test would you suggest I request my primary Dr &/or GI specialist do to confirm or rule out if I have Acute or Chronic pancreatitis? I had CT & ultrasound, Also, do you take digestive enzymes along with the supplements? If so, OTC or prescription? Local health food store suggested HCL with Pepsin.
Thank you & God Bless your ministry ??
Hi Peaches – sorry to hear you too have joined the pancreatitis hall of pain. I am guessing from what you’ve shared that nobody seems to know why you had an acute pancreatitis attack. With your previous history of AP I would guess or at least hope that they again did blood work that checked your amylase and lipase levels. Usually if lipase isn’t elevated acute pancreatitis is ruled out in most cases. You could be experiencing residual symptoms. The damage may have been enough to cause minimal change CP. CT is a great test but sometimes misses minute damage. EUS (endoscopic ultrasound) is often better at showing minimal damage and diagnosing early stage CP.
I do take OTC enzymes. Super Enzymes by Now Foods which is one of the best OTC formulas. There are probably others that will do as well. Thank you for the kind words and God Bless you back. I wish you better health and times. 🙂
Thanks Healthy Guy. Well I know you’re not a MD but residual, minimal damage & early stage sounds hopeful that I too will be able to beat this as you have. I pray healing prayers for everyone experiencing any kind of pain & health issues.
GI dr said AP attack may have been from the bacterial infections. (Flu &/or UTI) but sometimes it’s just unknown. I have family history both grandmothers passed from digestive issues. Maternal had diabetes & gastritis (alcoholic) and Paternal had gallbladder removed, pancreatitis & pancreas cancer. I read there can be a genetic disposition.
My blood work showed:
1st hospitalization
Lipase Amylase
3/4 1721. 74
3/5. 388. 48
3/8. 248. 40
2nd hospitalization
3/22. 154. –
3/23. 123. 40
Yes, I had Ct scan, MRI & Ultrasound as in-patient and endoscopy & colonoscopy out-patient. Honestly, I must give you credit because in between my 1st and 2nd bout to the hospital is when I came across your blog while on Curezone. When my pains began to return after my 1st discharge, I started drinking the grapefruit juice & taking ibuprofen. Although I did end up going back to the ER just based on my lab results, my #’s were no where near what they were the 1st time, which I presume is why they said the 2nd time wasn’t pancreatitis. (wonder what the #’s would have been if I had not guzzled grapefruit juice & taken the ibuoropens ? nope don’t want to know)
What’s confusing is I had no warning signs the 1st time. I just woke up felt fine, went to the bathroom and then all hell broke lose. I literally stayed in there all day. Over 15 hours before I made it to the ER. The second time was this annoying, agitating tender pain, nausea and lose of appetite.
Since I was released the 2nd time I started taking your recommended supplements. I’m going to follow up again with my docs as well since although my pain it’s manageable the off & on discomfort is consistent. I guess due to not having a solid hold on my diet do’s and don’t. Since my OOP deductible is $7K, I may as well have them monitor me regularly like a hawk & do every darn test that’s out there to rule out and confirm exactly what’s going on. Failed to mention test showed kidney stones. Too large to pass so will have to be removed one day. Kidney specialist said they are non obstructive and not the cause of my pains.
Many blessings & thanks again.
P.S. Would you ever consider starting a foundation? Love to see you partner with dedicated doctor(s), write books & have speaking engagements. You help shine such a bright light of awareness & education to this illness. ?
I feel for you Peaches “What’s confusing is I had no warning signs the 1st time. I just woke up felt fine, went to the bathroom and then all hell broke lose. I literally stayed in there all day. Over 15 hours before I made it to the ER.” Yes AP does come on fast. I’ve been there, done that. The only difference is that MY seven (7) ER docs didn’t have a clue about what was happening to me. I’m so glad to hear that most of the people who comment on this blog about their experiences have had MUCH better luck with ER physicains.
I hope you are feeling better now.
I wouldn’t even know how to start a foundation. I have no thoughts about a book, I am a horrible public speaker and get stage fright lol.
Thanks for your kind words 🙂
Hi, I am having my blood checked for lipase and amylase levels. Would they always be high or only after you eat? Would all foods trigger a pancreatic attack? I have back pain after I eat but it’s not severe and debilitating like you described – haven’t vomited. Perhaps I don’t have Pancreatitis, though it’s hard to know. What are somethings I could look into besides these enzyme tests? Thanks.
Hi Lukus – I’ll take each question and answer as best as I can.
1) “I am having my blood checked for lipase and amylase levels. Would they always be high or only after you eat?”
Typically amylase and lipase only elevate if there is inflammation present in the pancreas or if there is some other condition present that also causes them to elevate. They do NOT elevate simply because you eat nor are they always high.
2) “Would all foods trigger a pancreatic attack?”
No, not usually. Foods high in fat or alcohol are usually the foods that cause inflammation in a damaged pancreas and lead to an acute pancreatitis attack or a chronic pancreatitis flair. NOW, it is entirely possible that a usually safe food could become “the straw that breaks the camel’s back” and triggers the acute pancreatitis attack BUT (get this) …
That usually safe food would NOT normally trigger an attack or flair IF the pancreas was not already highly inflamed due to alcohol or high fat foods previously eaten. So do grapes cuase an acute attack? No. Do vegetables cause an acute attack? No. Do carrots and apples combined cause an acute attack? No. BUT the steak with mashed potatoes, gravy and cheese cake that was eaten previously sure could have set the pancreas inflammation in high gear and then the cucumbers in vinegar (safe) were “the straw that broke the camel’s back.” SO …
In essence it is theoretically possible for ANY food to trigger an attack but it is NOT likely unless a high degree of inflammation is already present and the fuse of the underlying bomb is very short.
3) “What are somethings I could look into besides these enzyme tests?”
IF the enzyme levels come back normal you should ask your doctor this question.
Good luck 🙂
Hi Lukus again, I have read more things on your blog. Makes me wonder. First let me back up to when it all started. Back in Oct of 2015 i started having a pain, a mere stitch in my side on my left side. It would come and go, more annoying than anything. Then it started happening more and more. I finally went to the doc, she said Pancreatitis. Ordered some enzymes tests, they came back normal. I kept having this pain like someone inflated a small balloon in my left side all the time. It got worse when I tried to eat and I had a beer. I came back tot eh doc, she said it was probably an ulcer. Put me on meds Omeprezole. Stupid me, I took them without having an endoscopy. I took the meds for 2 months, it wrecked my gut suppressing the stomach acid causing leaky gut and candida overgrowth – that’s a whole different issue. Anyway At someone point in December I have severe pain in my left side (thought it was an ulcer – an endoscopy later revealed no ulcer) went to the ER, the pain went straight through me to my back. I cried, i rarely do. I was given morphine etc. However they did an ultrasound on my abdomen, several different times (no indication of anything – or atlas they never mentioned it) I even had a contrast CT at one point. However that mysterious night that the pain came out of the blue makes me wonder. I changed my diet drastically mostly to heal my gut- i still eat meat (not as much and absolutely no junk food or alcohol anymore) and on occasion I have mild pain not sure what to think cause of the leaky gut causing IBS symptoms.
Im still scheduled to see my doc for another enzyme test but after reading your blog I’m not sure it would reveal anything unless it was really inflamed. Is it possible to have mild inflammation? Maybe I should do the diet and eliminate fat and see if the pain goes away.
Thoughts?
Hi Lukus – hey my thoughts are that if you went on the diet and your symptoms disappear your condition obviously responds to a diet low in fat. Now that could be liver disease, gallbaldder disease (however your pain is in the wrong spot for GB issues), the sphincter of oddi also causes abdominal issues that can be mild or very severe, including acute pancreatitis. Depending upon where the pain is exactly it could also be kidney stones or a spleen issue or IBS. so it is not an easy thing to pin point especially if nothing blaring shows on tests. USUALLY acute pancreatitis causes pancreatic enzymes (lipase, amylase and trypsin) to elevate. If both lipase and amylase are elevated that is almost a 100% guarantee that you have AP. Lipase elevation of 3x normal is considered enough to diagnose AP.
Hi health guy,
Can pancreatitis cause gastritis? Why would pantoprazole be helping me with my symptoms?
Thank you kindly
Stacey.
I don’t know Stacey, sorry. If pantoprazole helps that’s a good thing right?
i have never been diagnosed with pancreatitus but have suffered all the symtoms for the last 20 years.i am now 67 years old and am still suffering chronic pain. i have had ct and mri scans and endoscopy and all they tell me is that i have pancreatic atrophy which i think means my pancreas has shrunk!) yet they (doctors) have put me on morphine for the pain and i also take creon with every meal yet i can not get a proper diagnosis,i find that if i eat anything that includes fat i am ill and will be for 24hours. i am plodding on myself trying to find the way forward for my condition as the doctors have not been able to help my condition.i havent had a holiday for 10 years and feel really down as nobody seems able to help me.i came across your page and feel that if i follow a more strict diet i might be able to see some light but at the moment i cant plan anything as i dont know how ime going to be every day.ime just so fed up of feeling so poorly and feel ime getting no help from the doctors anymore.my only hope is after reading your articles i might find a way forward.
Hi William – 20 years without a diagnosis is a LONG time. And yes atrophy means your pancreas has shrunk which can happen as we age whether or not one has pancreatitis. What I’m wondering is why they put you on morphine for pain when often times diagnosed pancreatitis patients can’t get pain meds. The creon is also an interesting prescription. Have you been diagnosed with EPI? Or do you have an intestinal disorder that has caused malabsorption? I’m puzzled as to why you’d be prescribed these meds without some diagnosis that indicated an actual need.
hi mr health guy i was perscribed oral morphine and mst in 2009 when i was admitted to hospital with severe pain (unbearable) prior to this i was on tramadol but during bouts of severe pain it wasnt working i didnt ask or want to be put on morphine but it seemed the only solution to the pain i was suffering but i now find that i am now addicted to this and need to come off which is another probem i must face at the same time i had-had diarrhea for three months and it was only when i was given creon that the diarrhea stopped although i have never been diagnosed with pancreatitus i find if i stop them myn symtoms get worse.i do not have EPI as ive been told by the specialists and as i stated previously i have not been told i have pancreatitus either yet i seem to suffer all the symtoms.i do not seem to have any malabsorbption issues and after all the tests i have had the only diagnosis is IBS..I find that life is passing me by as i feel unwell most days and yet can not get a proper diagnosis.i was attending a pain clinic at my local hospital and the specialist there told me sometimes there are times when people can not get diagnosed.therefore at the moment i am in limbo.
William it sounds like you’ve definitely had some rough road. It also sounds like you have more rough road ahead. I am truly sorry you are having to go through your ordeal. I KNOW it sucks. I also do not know what to suggest as a possible solution except what I have already said in another comment.
hi mr health guy can i just add that is it possible for me to have chronic pancreatitus and not being diagnosed as such,
Hi William – sure it’s possible. ANYTHING is possible. There are forms of pancreatitis that can present FIRST with chronic pancreatitis type symptoms instead of acute and so likely go undiagnosed for years. But here’s the deal – and trust me – I KNOW how much of a pain in the tail, frustrating experience it is to be sick and have doctors look at you like you’re some kind of alien life form but get diagnosed. Find a doctor who can think on his/her feet and knows how to listen to his/her patients. I don’t care if you have to go through 14 like me. Get diagnosed with a concrete diagnosis that actually fits the symptoms and makes sense.
thanks for your advice mr health guy.i will see if i can find a doctor that will listen and understand what i am going through funny enough ! a doctor diagnosed me with chronic pancreatitus in 2010 and then changed his mind on my next visit.it certainly gets confusing for me .
I understand your confusion. Docs are funny little creatures lol
Hi HG
Have a new Dr he wants me to have a Hida scan. As you know I’ve not been diagnosed with pancreatitis because bloods and previous scans are normal. So dr wants to look at my gallbladder function. I never have pain on the right only the left and feel it radiate to my back with nausea. The catch is they want me to eat bacon and eggs the morning of the scan. Am petrified to say the least.
Stacey
Hi Stacey – dang that would scare me too! “I never have pain on the right only the left and feel it radiate to my back with nausea.” Hopefully you mentioned that to your doc? Being the pleasant kinda guy I am I’d have probably asked him/her “If it were you or your wife/husband/child and the pain was all left side instead of right side and sometimes the symptoms are really bad after ingesting high fat foods would you or would you have someone you dearly loved eat bacon and eggs for breakfast doc?”
my mother died after 6 weeks with undiagnosed severe acute pancreatitis she never got admitted to hospital even after seeing 7 gps and visiting er 3 weeks after onset . She experienced no pain. very little is mentioned in textbooks about painless ap but i read in one that a painless presentation may be a sign of serious and fatal diease.Do you know of whether this is true.
stephen johnston – sorry to hear about your mom. I have a case study somewhere about an old man who presented with severe vomiting but no pain and he died. Diagnosis was on autopsy. IF I can find it in all my files I’ll link it to you. So yes I have heard of painless acute pancreatitis. Painless acute pancreatitis is rare and usually ends up fatal because the hallmark clinical symptom (pain) is not evident and so it rarely gets diagnosed in time.
Painless acute pancreatitis mimicking pancreatic carcinoma
Hello! I’m 22 and I’ve been suffering since May with severe epigastric pain (centre and left side under rib cage) and occasionally around my navel too. It is tender and feels swollen. Sometimes have 1 bad day 1 good, interspersed with a few weeks of awful. I don’t think gastroenterologist has even considered chronic pancreatitis as an option but i’m wondering if it is a possibility. I have had 2 CTs, an ultrasound and too many blood tests to count! All have come back normal apart from most recently had CRP levels of 80, raised ESR and slight neutrophilia. Have had 2 lots of fevers during this time which have lasted about 4-5 days. The pain appears unrelated to food but hard to tell! I haven’t had a drink since May so I’m not sure if alcohol has an effect, but I didn’t drink to excess before then. Celiac and autoimmune have all been ruled out- currently testing for Crohns. I was just wondering about the chances of having chronic pancreatitis having never had any pancreatic problems previously? Thank you for your time 🙂
Hi Lu – sorry to hear you are not well. All I can say is that there is definitely inflammation somewhere because your CRP is elevated which clearly indicates inflammation. The only problem with the CRP test is that it doesn’t tell where that inflammating currently resides however … acute and chronic pancreatitis both elevate CRP. Not saying you have either but with your symptoms I wouldn’t rule it out even IF your enzymes did not elevate. Yet, it isn’t common to have acute pancreatitis without amylase and lipase elevation. Neutrophilia could be indictive of any number of infections, even though slight. There are certain types of pancreatitis that can start out with symptms more like those a the chronic form. Have you done any genetic testing for hereditary or acoholic pancreatitis? You do NOT have to be an alcoholic or even a heavy drinker to get alcoholic pancreatitis if you have the gene varaiant. Sorry I am not more help. 🙂
Hi Health Guy.
I hope you’re well and keeping healthy, for both your sake and that of everyone in need of this website.
If possible, I’d like to get your opinion on my situation. I’ve had ongoing upper abdominal pain for about 2 years (mild, but worse after eating – especially after the common triggers). The discomfort is dead center in my upper abdomen, and does not radiate to my back. Undiagnosed, as all GI tests came back normal. This was triggered after a night of binge drinking (10+ drinks), and the onset was quite gradual. I did binge drink regularly in university (3-4 times/month), but it wasn’t out of the ordinary among my friends. Frequent diarrhea/soft stools in recent months.
Here’s my question – have you come across any chronic cases with such a mild onset? I’ve never been hospitalized/had an acute attack the past. I’m not drinking anymore, but I did continue to drink socially for the past 2 years (1-2 times/month).
If you’re able to respond, thank you in advance. Any information is appreciated!
Nate
Hi Nate – I can’t diagnose, I am not a doc. Now that I’ve said that … it can be that one who has the genetic variant that predisposes them to alcoholic pancreatitis, which can present as chronic first, is a possibility. And if one has the genetic variant there isn’t a need to be an actual alcoholic, regular or binge. SOD (sphincter of oddi dysfunction) can present with very similar symptoms to acute pancreatitis and does actually cause pancreatitis. It could be neither yet is a harbinger of things to come. I know that is really VAGUE. I’m sorry I am not more help.
Hi Health Guy. I have abdominal pain radiating to my back especially after food, soft stools, dizziness and have seen a number of doctors. I have had a CT scan, two MRI Scans and an ultrasound endoscopy and they have all come back saying my pancreas looks normal. My bloods are also normal. I was told the ultrasound endoscopy would definitely show if I had a problem with my pancreas. Is it possible to have chronic pancreatitis when all the tests have come normal? I am also worried I have malabsorption issues as my bones have begun to hurt a lot and I am wondering whether undiagnosed pancreatitis has resulted in osteoporosis. Is there anything you would suggest for malabsorption other than juicing which I am trying to do as much as possible.
Hi Jen – The problem is that there are more than one condition that offer those types of symptoms. Your pancreas may or may not be involved. Endoscopic ultrasound is a very good test. I’d be more inclined to look in other areas such as gallbladder inflammation (inflammation, stones, sludge) or sphincter of oddi dysfunction both of which can also cause similar symptoms as those seen in pancreatitis. Both of those conditions can cause acute pancreatitis as well. Yet with the tests you have had a gallbladder issue may have already been ruled out. SOD can also be seen (not always) on those tests. Keep in mind radiology tests are only as good as those performing and /or reading the results. Things sometimes get missed. Gallstones can pass leaving nothing to be seen. SOD doesn’t always show up via radiology tests. Blood enzyme levels have been known to be elusive (rare). And if you weren’t currently ill when those tests were performed inflammation may not have been present at that time. Tests aren’t perfect. I’d continue to pursue a diagnosis. Obviously you have something (what it is I don’t know) going on which isn’t simply showing up for some reason.
Thank you Health Guy. SOD has been ruled out but I have also had a Hida Scan and that showed a sluggish gallbladder. Could that be responsible for my symptoms?
Hi Jen – I THINK (I hate the words I think cuz it really means I am not sure or don’t know) a sluggish gallbladder could contribute to your symptoms. It may not empty properly which leaves stagnant bile that could form stones that pass and cause problems (symptoms) but don’t show on scans because they are no longer there (they have passed). In order to help resolve the “sluggish” gallbladder and stagnant bile I’d drink plenty of water.
I’d also detox my liver.
Bile is made in the liver and stored in the gallbladder. If your liver is toxic the bile probably is as well. Good liver cleansing herbs are mint, parsley, garlic, chives, shallots, basil, coriander and small amounts of thyme and oregano. I’d also do raw juicing with cabbage, carrot, ginger root, mint and apple. I’d also eat my vegetables raw as much as possible. I’d also get some milk thistle (supplement) and take it once a day for a week and then work up to two per day. IF that is gonna work you should see some results within 30 days.
Do you think getting my gallbladder removed would result in a lessening of my symptoms? Thank you so much for your help. I seem to get better advice from you than the consultants I have seen!
Hi Jen – I can’t advise on that because I don’t know. Plus about 30% of people who have their GB removed still have pain. There are times when the GB should probably be removed but I don’t think (from what you have said) your tests indicate that; however, that does not mean I am right. Oh and I’d avoid high fat foods and junk (chips, etc).
Hey Healthy Guy, I know you’re not a doctor. I just hope that maybe you came across with someone who had similar sympthoms in the past & can help me with my situation.
My name is Ori (age 32) and i didn’t got diagnosed with anything yet but I’m worried that I have early symptoms of chronic pancreatitis. It started 4 months ago when I drank about 7-8 glasses of whisky and went to sleep an hour later (I don’t drink all the time but when I do, this is the amount). When I woke up I had a pain / burning sensation under my left rib and I felt the place beats / pounds strongly. It wasn’t a crazy pain that a man can’t tolerate, but I went to the doctor, he basically said not to worry about it. After a week or so the pain slowly started to go away and turned into a mild, but constant burning sensation under left rib and in upper stomach in general. For the last 4 months I’ve lost 15 Lb in weight and my stools aren’t looking healthy (looks like clay with tiny pieces of food in it). If I eat really big meals or junk food it may comes out in a diariha shape. Sometimes I have mild twiches / spasms in my stomach.
After couple of good blood tests and a normal Ultrasound, two of my doctors said that my pain isn’t a reflection of anything related to CP. When I suggest a CT or MRI they said “no need”. After researching online like crazy, I was affraid that I’m causing more damage to my pancreas so 3 months ago I went on a diet till this day (no fat, no alcohol, no sugar, etc). The sympthoms are still there. Again, I understand you are not a doctor but from what I see online for the las months you have more info than most of them! Do you have any advice for me? What do you think?
Hi Ori – sorry you aren’t well. I know it can be frustrating to be ill and not know why. I also know that what I’m going to say isn’t necessarily what you want to hear but you need to get diagnosed. From what you have said I’m guessing that nobody knows what is causing your symptoms. Did the docs check you for celiac disease or IBS? Were you ever in the ER? If so … Did they draw blood and check your lipase and amylase levels? It may not be pancreatitis. It may be an intestinal or liver problem (left lobe). Did they check your heart (you mentioned beats/pounds strongly)?
Hi Health Guy thank you for the response. I know that i have to get diagnosed but i feel like the docs don’t listen to the problem. 4-5 months ago i had a burning pain under my left rib after drinking a lot of whiskey and still have that pain (lighter) till this day. I’m 100% sure that’s the thing that started this or at least the last straw – they say its a coincidence. I heard stories about people that had mild symptoms for years and than one day their pancreas was so damaged they needed to remove it completely. So i’m trying to get a picture of early symptoms to a damaged pancreas. If that is the case with me, i want to make a change before its too late.. That’s why i’m here to see if someone can help me by telling me a similar story.
Here are my symptoms one-by-one in case anyone is familiar with them:
1. pain / burning sensation under left rib after alcohol (about a week).
2. constant burning sensation under left rib (till now).
3. pale stools – clay color (constantly).
4. weight loss.
5. spasms in weird places (stomach, leg, arm, right waist).
The answers to your questions:
1. The docs didn’t mention celiac as an option so i guess the symptoms don’t fit.
2. After 4-5 months that my doc tells me i’m imagining and i’m ok, he told me yesterday it may be IBS and gave me pills for that (don’t think the symptoms match).
3. Never been to the ER because the pain was and still tolerable.
4. Ultrasound & Blood test was normal when i did it 2 months ago including lipase + amylase.
5. I was told it can’t be the liver because the blood tests are normal.
5. EKG check showed everything is fine with the heart, but the pounds/beats i’m referring to are NOT from the heart. They are from the stomach, mostly from the place of the burning pain – under my left rib.
I hope my answers are good enough to describe my situation so you can give me your opinion..
Ori – let me quote you “After 4-5 months that my doc tells me i’m imagining and i’m ok, he told me yesterday it may be IBS and gave me pills for that (don’t think the symptoms match).” It is interesting to note that your doc thinks you have IBS. Just for giggles and grins have him test you for celiac disease (blood test). Read this whole article from the Cleveland Clinic. IF it isn’t celiac disease you’ve eliminated one possibility. By the way – go to the store and buy some Mylanta (antacid). Take a dose twice a day for a couple days and see if that burning pain goes away. If it does it could indicate an ulcer, or a problem with your esophagus. I had esophagus pain (left and right side) that feels like it is something other than the esophagus that was relieved by Mylanta. I also had reflux at times.
Check list
By the way – even though most of your symptoms do NOT indicate pancreatitis as yet they may be signs of things to come. Knowing what I now know IF it were me I’d quit drinking too.
Ok, I will take this advice. Again, Thank you.
You are most welcome!
Hi Health Guy
Drs are now starting to finally think I have chronic pancreatitis after 10 months of exhausting all other tests for different things (not to mention the small fortune that I’ve paid for them). My specialist wants me to try taking Creon to see if that’s helps. Creon scares me a bit though I think I’d prefer to take the natural ones. But I do know this, following your regime definitely helps me and it’s the only thing I believe that has kept me out of hospital for the last 9 months since I’ve been doing it. I have dropped my grape seed extract for now because the milligrams I feel were way too high. So I’m going to order the ones you recommend. I need to keep reading and visiting the beatingpancreatitis website because importantly for my state of mind I need hope. Hope that I can heal too. I can’t tell you how thankful I am that you keep this website going. God bless.
Hi Stacey Wykes – I was just asking the Lord yesterday about you! I mentioned to Him that I had not heard from you and asked that He made sure you were ok. You can always try the Now Foods Super Enzymes. They might be enough to give relief (start with one at each meal and work up if one isn’t enough). IF your insurance covers the Creon (it’s pricey stuff) then by all means give it a try like your specialist suggests. It may give you the relief you need. Just ask the doc to start you off with a low dose and see what happens. In regards to hope here’s what I think: “Jesus looked at them and said, “With man this is impossible, but with God all things are possible.” – Matthew 19:26
Such a great quote from the bible and very true. Because of your good work and wonderful effort I think God led me to your website very early in my illness and for that I am so grateful. I have left a couple of messages but they mustn’t of made it to you or I haven’t been getting the email notifications when you reply – not sure. Anyhow I will see my dr tomorrow check the creon dosage is low and then try them. If it helps that’s a plus. I’m going to organise myself this week with all the proper supplements and juicing. I feel ok (am still following the diet) not as good as I know I can so I need to get myself organised. Need to get the inflammation under control and do my food diary. I’m going to leave you a few questions in food topic if that’s okay?
Thank you for caring, your a gem ?
Of course questions are fine Stacey. I hope you begin healing and feeling better 🙂
Hi HG.
I’m not getting email notifications when you reply. Pancreas is not inflamed at present ? as long as I stick to no fat (after what I’ve been through I wouldn’t touch alcohol with a ten foot pole). My diet is pretty yummy these days despite fat free and vegan ?. So there’s hope there for anyone reading this and feeling over whelmed it just takes some adjusting. You can do it!
Hi Stacey – weird, maybe something happened when I deleted all the forum sign ups. Glad to hear you are feeling better!
Hello Healthy Guy, I really enjoyed your blog, I think I have chronic pancreatitis and Im so upset by it because other websites and forums only say I will suffer and die soon :/ I have my symptoms for almost a year and I underwent all tests including EUS which showed hyperechoic wall in my head of pancreatic duct which for doctor is not and evidence to make CP diagnosis, I never had acute attack and Im scared I will every day, I have bloating and feeling full after eating, lost weight and sometimes my stools are not the right colour ( a bit lighter or yellow ) symptoms are very annoying, I dont have any typical pain and never had ( more feeling of swollen upper abdomen and lower) but last year I was depressed and did drink a bit too much like 2-3 beers a week. I also used to be a party animal on university. My stomach and intestines are ok, my stool tests showed single fat drops, I dont know what to think about it, this constant indigestion is so annoying also Creon sometimes helps and sometimes not ( I can eat fat steak and feel ok with no Creon and have problem with light food) I never felt bad after alcohol, however my symptoms started after eating bad fish, I am so worried… :/
Hi Kate – sorry I have taken so long to reply. Why were you prescribed Creon? Someone (a doc) thinks you have something going on. Did they mention any diagnosis? I know the concern you have but it isn’t good to live in fear. You may want to consider giving up alcohol. I’ll await your reply.
Thank you so much for your reply! No one prescribed me Creon I am taking it myself, here doctors think when you have good amylase and ultrasound you dont have pancreas issues so I had to make all tests myself and pay a lot for them. They have excluded all other diseases so its obvious to me I have CP. Just when I understood this I stopped drinking even it never gave me any issues so no alcohol for almost a year. I am so tired going to sleep with upset stomach and wake up with it and so scared of whats in front of me with this disease… 🙁 Every food caue indigestion and stomach swelling even Im on low fat diet, I take curcumin and grape seed extract since few days. I am shocked its alcohol I always thought you get AP first and also every source say you need to drink heavily for at least few years is that true? I thought few beers a week are not too much, my friends drink every night a coctail or wine for years and are fine I have lots of friends and dont know any person with CP not even AP…:(
Hi Kate – I have never heard of being able to prescribe Creon for one’s self or getting it over-the-counter without a prescription. That is interesting! Your country must be quite liberal in regards to tests and drugs. I know this isn’t what you want to hear but there are a myriad of diseases/conditions that cause nausea, vomiting, indigestion etc other than chronic pancreatitis so CP is never an obvious diagnosis. Even good doctors have difficulty diagnosing CP, even in patients who have suffered acute pancreatitis previously and display damage on tests.
Just as an example I have celiac disease as well as pancreatitis. Celiac disease by itself can cause nausea, vomiting, indigestion, bloating, diarrhea and many, many more symptoms. Beer is full of gluten and so would trigger symptoms in celiacs. It could be another form of IBD such as Crohn’s. It could be liver disease or any number of other conditions. BUT with that said …
Alcoholic pancreatitis often presents with mild CP type symptoms first and you do not have to be an alcoholic. IF you have the genetic variant (only genetic testing can confirm the variant) that predisposes one to alcoholic pancreatitis social drinking can be more than enough to trigger the condition. You may want to pursue a proper diagnosis especially if you find no relief from diet coupled with the curcumin and grape seed extract within a few weeks. I wish you better health in the future.
Dear Healthy guy! Thank you again for your response, we dont need prescription for Creon here unless is not a huge dose, do you think its harmful to take 20 thousand units pear meal? Some doctors said I should do it others say dont. I am confused, I do know that many diseases mimic CP. My EUS showed a little bit more visible wall in the duct in head of pancreas, doctor was not able to answer if this is normal or already start of CP, I also couldnt find info if some cp findings except from calcification which are obvious can be present in normal pancreas. Also do you know what variant is it I could check? The SPINK gene? And my last question is by mild CP symptoms of chronic alcoholic CP you mean some small indigestion or pain or discomfort after consuming alcohol for example? I had no issue wit it even when I drank some beers having symptoms of what I thought was stomach problems. Sorry for bothering you so much but I know u did a lot of research 🙂 I did all tests like gastro and colonoscopy ct 3 mri mrcp eus celiac hepatitis parasites – all negative 🙁 I didnt do test for SIBO and Hida Scan, maybe I should? Regards!!
Hi Kate – IF Creon isn’t necessary why take it? But you should ask the doctor you trust most why he/she thinks you either need it or don’t need it and go from there. This post has a link to another article that mentions the genetic variant. Yes, by mild CP symptoms I mean indigestion, nausea, pain after eating or drinking alcohol. Those mild symptoms could escalate into something far worse if you do have mild CP. I hope you find out what the problem is so it can be resolved.
Thank you for your blog. I 100% agree with you that the doctors have offered horrible advice and have no clue on how to treat pancreatitis. When I tell a doctor that I have had pancreatitis they don’t even believe me (I first was diagnosed early 20s white female and didn’t fit the statistic). I have had it my entire life – drugs, other illnesses, food are all triggers. Tamiflu is horrible…now I know. I think your blog is really helpful and honest even when I don’t want to hear the advice. It has gotten progressively worse as I have gotten older (now mid 30s) – I use to be able to eat/ drink whatever and only got sick once every 3-4 years but now I am a lot more sensitive. But I do have few questions are 1) have you had any experience with aloe vera juice? I have found this to be a life saver for me in stopping the pain; 2) I have not had the same experience with you with coffee. I admit that the only times I noticed a direct correlation with coffee and pancreatitis was when I was pregnant but I am 100% sure the two are linked. Again, I was pregnant so maybe that changed some of the facts. Have you heard that from anyone else? 3) I have found I can tolerate fat- coconut, olive oil, almonds, avocado, salmon. I agree red meats, dairy are out. And gluten I think but not 100% sure gluten and the pancreas don’t mix. Do you think there is a spectrum?
Hi Christine – you and I were diagnosed about the same age. I was 25. However my first symptoms showed up when I was 19 (misdiagnosed as usual). Anyway I am sorry you have to deal with pancreatitis. Now to answer your questions …
Question 1) “have you had any experience with aloe vera juice? I have found this to be a life saver for me in stopping the pain.”
Answer: It is funny you should ask (great question by the way) because another reader asked me a few days ago about aloe vera juice and said the same thing you have that it helped eliminate her pain. I tried it years ago. It was a product offered by Forever Living. It tasted like dung. So I never gave it a good try. I have never been able to find any good science regarding the efficacy of aloe vera juice in pancreatitis but like I said you are the second lady to ask and vouch for it so … all I can say is if it works keep using it!
Question 2) I have not had the same experience with you with coffee. I admit that the only times I noticed a direct correlation with coffee and pancreatitis was when I was pregnant but I am 100% sure the two are linked. Again, I was pregnant so maybe that changed some of the facts. Have you heard that from anyone else?
Answer: No BUT … You said this “I use to be able to eat/ drink whatever and only got sick once every 3-4 years” so unless you have completely stopped eating what I call trigger foods there really isn’t a way to pinpoint the actual cause as coffee. Trigger foods such as red meat, pork, lamb, duck and other high fat foods (mayo, egg yolks, nuts, avocado, coconut, butter, margarine, cream, whole milk, cheese and more) eaten by people who are told they can eat a “normal” diet do NOT always cause immediate (1-6 hours) discomfort, flairs or acute attacks. I can’t tell you how often I have had people tell me who are still eating a normal or near normal diet tell me that grapes (super anti-inflammatory) caused an attack yet what really caused their attack was the roast beef, mashed potatoes and gravy they had on Sunday at grandmas (two days ago) that came on after eating the innocent grapes so they blamed the grapes (or beans, or cabbage, or whatever is almost always safe) instead of the good tasting food they didn’t want to think of giving up. In fact there is only one way to actually know for sure what does and does not cause you pain or even an acute attack and that is by following my food diary prep and then actually doing a food diary by adding one food at a time and eating it for a certain amount of time (depending upon whether plant or animal in origin).
Question 3) I have found I can tolerate fat- coconut, olive oil, almonds, avocado, salmon. I agree red meats, dairy are out. And gluten I think but not 100% sure gluten and the pancreas don’t mix. Do you think there is a spectrum?
Answer: You can tolerate far more food than me. Now 10-15 years ago I could tolerate a lot more fat than I can now. Then I screwed up and ate some food I shouldn’t have eaten once let alone 3 times in one week and I had one of the worst acute attacks of my life. I was very sick for 12 days (I even filled the toilet with blood once) and was sick for another 4 weeks or so after. That was the beginning of the less toleration of fat. There is definitely a spectrum in regards to tolerated foods (amounts of fat) and that seems to vary from person to person depending upon damage. Gluten shouldn’t be an issue unless you are a confirmed celiac (like me lol)
Dear Healthy Guy! Its me again 🙂 I still have no diagnosis, for the moment my indigestion is a bit smaller but I have issues with my stool, its a bit yellow/green often and looks greasy. But I have no pain no nausea and can eat what I want ( some fullness afer food) I take enzymes from US company, I am so confused… oh and I dont really put much on weight, I am able to put just one kg and then it goes away quickly. There is no logic in my symptoms at all… 🙁 Is there any other pancreas disease that could go away after time like a dysfuncion or something? All other diseases excluded :/ regards!!!
Hi Kate – what exactly are your symptoms and when do you notice them most?
Healthy Guy for the moment they are: bloating and full after food, this start around half hour after eating and last around hour. In the morning I have to go to bathroom quite fast, stools are rather normal except awful colour ( yelllow,green,gray,clay,pale) and often I have white specks ( no parasites) weight loss that I cant get back, I feel awful after lactose, I tolerate meat the best, I feel tight muscles of stomach and intestines – cant call it pain its discomfort.
Kate – you said “I feel awful after lactose” so quite drinking milk, eating cheese, cottage cheese or any dairy including yogurt, ice cream, and butter. ALL contain lactose. Try fat free, lactose free milk and see if that works. Lactaid makes a lactose free cottage cheese. See if your symptoms subside.
Hi There,
First love that you are helping and sharing your knowledge with so many people. I am sure that you are helping many people so thank you.
I am deciding on whether I should see another specialist. I have seen 3 GI specialists and one chronic pain specialist.
I have had epigastric pain for a little over a year now. I have rheumatoid arthritis and was on pretty strong medication at the time. I started having bouts of diarrhoea so I stopped the medication. I celebrated a couple of 50 birthdays and drank probably a little too much (bottle of wine) and have enjoyed a few glasses several times a week of wine over the past 10 years. The diarrhoea stopped and my stools have been normal for the past year. I developed pain in my epigastric area which hasn’t gone away. I don’t suffer from nausea or any other symptoms which the exception of foul smelling gas from time to time and a noisy high pitched whistle coming from my stomach. At the time I became sick I lost 7 kilos in weight as food wasn’t my friend and was very stressed through worry. I have since put all this weight back on plus more as they put me on antidepressants to help with my pain so have no problem eating. I have continued to have my few glasses of wine throughout the week in which my pain does change if fact it probably relaxes things and makes me feel better. My pain isn’t relieved from leaning forward…it actually hurts more and with exercise it becomes worse. I see a chiropractor weekly which helps manage my pain and he always notes that my diagram is stressed.
I have had every test which all tell me I am a picture of perfect health with the exception of a 0.5 mm cyst on my pancreas which no one is concerned about.
1 x ultrasound
1 x Ct scan with contrast (adominal and chest)
2 x Mrcp (one when I first developed symptoms and another 6 months later)
1 x hida scan
1 x bone scan
2 x upper gastroscopy
1 x colonoscopy
1 x stomach emptying test
1 x exploratory laparoscope
I have had blood tests every month for my RA where they have all been perfect and since I have been in pain they have down further checks and have checked my amylase and lipsase have all been normal.
All my specialists including two GPS have diagnosed with with a functional abdominal disorder (not ibs though as I don’t have problems with bowels).
I am becoming quite depressed with this pain and not really sure if I should be accepting this diagnoses. The problem is that as they feel that there is no evidence to suggest chronic pancreatitis that in their opinion is most certainly isn’t and that it is well and truly ruled out. They says that I should have something either in my lords or scans.
Do you think I have done everything to rule it out? The problem is that when I go to the doctors they look at me as because I look well and manage my pain they think I can’t possibly be that sick.
I am sorry for the long post but I thought that reaching out to you you maybe able to either put my mind at rest and accept my diagnoses or tell me to continue to explore the chronic pancreatitis path.
Thank you for taking the time to read my post.
Regards
Karen
Hi Karen – thank for the kind words. Don’t apologize for the length of the post. I did see you have two of the same so I only approved this one because google doesn’t like duplicate content. Anyway … you have had a lot of tests and they have obviously looked for signs of cancer (exploratory and bone scan etc). I don’t know how much you have researched pancreatic cysts but there are two types pseudocysts (inflammatory cysts) and true cysts (non-inflammatory cysts). Often doctors can’t figure out why a cyst (especially a true cyst) is there and so may seem unconcerned, may even be unconcerned yet … I am under the opinion (and it is my opinion only and I’m not a doctor or scientist) that a cyst (of any kind) is not simply an extra piece of equipment such as would be ordered on a car or truck. In fact God did NOT design the pancreas with cysts as optional equipment so it is there for a reason. And from what you have explained I’d guess it is the reason you are experiencing the symptoms you have. If you haven’t done research here are a couple sites you should read thoroughly and begin your learning process – not to scare yourself to death but to become as informed and learned as possible. Having information helps you to know what questions to ask your doctors (WHY is it there? What is your plan of action? etc).
Pancreatic cysts
Pancreatic cysts (Mayo)
Pancreatic Cysts and Pseudocysts
Many thanks for your reply. I will certainly be doing some reading. I had asked the GI specialist and my doctor what that’s means and they have both said it is very common to have small cysts show up on scans. My cyst is 1/2 mm. I also asked whether I should follow up with scans down the track and they both said not necessary. so does this suggest that I may have had an acute attack of pancreatitis or have chronic pancreatitis? All doctors have told me that I would be in a lot more pain than what I am in and that it is functional…sigh.
Thanks again for your help, very much appreciated.
Karen
Karen – there may be no reason to be concerned but I often wonder if the doctors had the cyst, instead of you the patient, how would they then approach the situation. All I can say is if your symptoms change or get worse make sure you get checked out again.
Hey Health guy I commented on another post but I had to share this! Not sure if you’ve come across this article but it suggests the potential to actually regenerate pancreatic cells with these treatments.
https://cdn.intechopen.com/pdfs-wm/47346.pdf
Wishing you well. A fellow brother in Christ.
Hey Brandon – great article! And one I haven’t read before 🙂 I know pancreatic acinar cells can regenerate. There are a couple of articles out there that testify to that fact but I hadn’t read about pancreatic stem cells. I’ll have to read that again. Thanks, good stuff 🙂
If I have had an MRI with contrast which showed no inflammation of the pancreas, does that mean I am in the clear.
I don’t know Evelyn. Sounds good, how do you feel?
Hello Health Guy,
I just wanted to wish you a Happy New Year. I pray all of God’s blessings & promises be unto you. Wisdom, knowledge, good fortune & health. Thank you for sharing & thank you for helping me. I am approaching 2 years and all of my test continue to come back great. Also, I am symptom & pain free as I subscribe to your low fat eating lifestyle. Continual Blessings to you & yours.
Ms. Peaches
THANK YOU! Ms. Peaches 🙂 Happy New Year and God’s blessing to you as well. It is awesome to hear of your success. I am so glad to hear you are feeling much better. That is great! Symptom and pain free is a wonderful blessing. God is AWESOME! Praise the Lord 🙂
Hello Health Guy,
My name isKimberly and much like everyone else my pain started in my abdomen just under the rib cage and slightly to the left. GI started off with GI and then colonoscopy- both were normal. I also had a traditional ultrasound and CT with and without contrast. So far everything has come back normal.
After all cleaning associates with the colonoscopy I suddenly felt better. I thought “looks like all I needed was a good detox”. Had a glass of wine that night then the pain returned with a vengeance! Pain is now in my back and feels like I’m being stabbed when I lay down so I only sleep on my right side.
I have stopped eating meat. The other day I had some white fish and it came through undigested in the stool. Salmon made me feel terrible! So now I’m vegetarian.
I believe I have a case of early chronic pancreatitis. I’ve been dismissed by my GI (he said it was arthritis in my ribs) and my primary care doc said something about intestinal cilia not working. Both I feel are utterly ridiculous. What test should I demand that will help confirm or rule out my suspicion?
Thank you so much!
Kimberly
Hi Kimberly – sorry to hear you are not feeling well. If you can go to urgent care or an ER the next time you feel real lousy and ask for them to test your amylase and lipase (pancreatic enzymes). That would be first step and if your lipase is high that will indicate what needs to be done next (more testing).
Hi Health Guy, I’m a concerned dad with a 20 year old daughter that has symptoms very similar to those noted above. Mid upper gastric pain which is almost continuous, even to the point of waking her up at night. Just like the others all tests have come back normal the majority of the time. We have seen Doctors from New Orleans to Houston to North Carolina. She has had multiple scopes done from both directions along with MRI’s, MRCP’s CT scans, Laproscopy, Ultrasound, including endoscopic ultrasound, Hida scans, thought it was the gall bladder and had it taken out, no change in the pain. The Gastros just kind of throw their hands up. Shes now going to a pain management Dr who has tried injections at various sights to try to determine where its coming from. Hes had very little success. The reason I think it may be CP is the overall progress of the symptoms. Started when she was about 8 yrs old, She would complain of stomach ache immediately after eating but it would pass in a few minutes. Then at 14 she had a spell that lasted hours and we ended up in the ER. This has gotten progressively worse to where its constant with a higher level if she eats anything. Many ER visits hospitilizations and dr visits later and we still dont have an answer. Shes basically living on pain meds. Also seen multiple counselers and a phsyciatrist or two, at the drs urging, because it must be in her head.
So my question is do you know of any top notch Drs. that are good investigative diagnostitions?
Have you ever been treated for Sphincter of Odi Dysfunction? Do you think that could be a possible cause?
Thanks for your advice
David – concerned dad – brother in Christ
Hi David – sorry to hear about your daughter. I have been hearing that more and more people are actually being diagnosed quickly (wasn’t my experience) so many docs are recognizing the symptoms in patients and maybe learning to listen better too but that doesn’t mean your daughter hasn’t had some docs like I had. But when I did get a good one he diagnosed me and things improved. It sure does sound like she has had all the right tests. AND that would be really frustrating. I was thinking sphincter of oddi dysfunction before I got to the end of your post where you asked about it. I have never been treated for it but IF that is the problem narcotics can often make it worse. SOD is difficult to diagnose and the tests to measure sphincter pressure can have unwanted to dangerous complications. There are 3 classes of SOD, 1, 11, 111. 1 & 11 are usually the worst regarding symptoms. “Type I patients have pain as well as abnormal liver enzymes and a dilated common bile duct. Type II SOD consists of pain and only one objective finding, and Type III consists of biliary pain only.” Sphincter of Oddi dysfunction: Managing the patient with chronic biliary pain Here’s a Google list of articles from decent sources about SOD.
Unfortunately there are very few great pancreas doctors. Google david whitcomb md pittsburgh. He is one of the best. You might also check out the Cleveland Clinic or Mayo Clinic. I wish I could be more help.
MOST digestive disease responds to diet. Pancreas, gallbladder and SOD respond to LOW, NO fat diets. They also respond to anti inflammatory drugs like Ibuprofen because they all consist of inflammation. Grape seed extract (highly anti inflammatory) and vitamin C work hand in hand to reduce inflammation. But it would be nice to know what her condition actually is so persist in finding a diagnosis. I’ll pray that God helps you find a good doc and even heals her. Keep the faith – “faith comes by hearing and hearing by the word of God.”
To Health Guy
Thanks for your blog. It’s well done and thoughtful.
I have had some GI incidents in the past four years. C-diff four years ago, and then a strange cessation of motility three years ago, as soon as I got to Asia for a two month stay. I had to push my stools out every few days and they seems continuous, not discrete. That situation resolved after a month or two of returning without any attention..
Fast forward to six weeks ago. Explosive diarrhea for one day, then less severe diarrhea for two weeks, then constipation for several weeks with very small, light brown stools. Also fatigue, and mild nausea. Mild pain in back, gas. Fast forward to this week. Normal stools returned, nausea and fatigue subsided. A week or ago, a GI doc diagnosed me has having ‘resolving pancreatitis. He made that diagnose with blood work (75 lipase, a bit above normal range, and a CT scan that showed nothing unusual with the panaceas or any other organs.. Based on your blog, I have been on a modified liquid diet for a week or so which seems to be helping. I had some mild pain in my back and sides but that’s getting better. Some mild bloating and gas also. The doc never gave me a diagnosis of either acute or chronic pancreatitis. Just ‘resolving’. I never had the extreme symptoms described for acute pancreatitis. And I’m not suffering much now, if at all. Mild symptoms. But eating very carefully (a modified liquid diet — soups, non-fat, fruit smoothies with almond mild, fresh fruit) The doc said I should return to normal in time (didn’t say how long) with low fat diet and no drinking (most likely the cause of all this).I quit two months ago, just before this whole thing started. Is there such a thing as a pancreatitis that isn’t either chronic or acute, just a relative minor inflammation of the pancreas? Possible or no? I’m tempted to go to Mayo Clinic for a second opinion tho I know from personal experience they aren’t always as expert and they advertise. Opinions?
Hi Rob – sorry to hear you have been ill. I’ve never heard of resolving pancreatitis yet your doc may have been thinking that you experienced a very mild attack of acute pancreatitis and the inflammation was/is resolving. In other words you may have had some very mild inflammation in the pancreas which is getting better. C-diff isn’t fun and can in fact be very dangerous. I know a gal who visits this blog and she has it and has a BAD case. So bad she was scheduled for surgery to remove some of her intestines. I haven’t heard from her in awhile so I am praying she is ok. Sometimes it is good to get second opinions.
Health Guy
Thx so much for your thoughts. I am basically doing what you suggest regardless of what I have or don’t have. I am still susceptible to too much food, even non-fat food, as I discovered last night when family visited. I went from basically a liquid diet to a full meal and it was too much. Mild upset of stomach, slight loose stool following. I am going to be very careful, with vitamins, for six months to see how things progress (or don’t).
A big benefit of this diet is my cholesterol which I have watched, but not carefully enough, since I got a coronary stent five years ago. Unless I have congenital high cholesterol, this diet should help me. I actually feel better without sat fat. Lighter.
I will probably be back in touch with you if things go awry.
Thanks again. You really do provide information which I can assure you (since I research things extensively) isn’t available anywhere.
Rob Furlong, Prescott, AZ
Hi Rob – I am sure your medical team will discover the problem. Hang in there. I’m glad you like the info on this site. Thank you for your kind words. Feel free to ask any question and I’ll do my best to answer, however, if I do not know I won’t try to snow you. Good luck! 🙂
Health Guy
I answered your very appreciated advice/opinion but my reply didn’t appear in the string so I’m doing it again.
If your speculation about what my doc is thinking, and that is in fact is the case, what course would recommend for me supplement-wise and general diet-wise. I’d like a minimum regimen to start since I’m not good at keeping track of too many things at the same time (I’m 77 with declining sharpness). If it proves insufficient, I can always up the ante. So which vitamins are vital, in what dosages, and what foods are absolute non-no’s.I know about alcohol. Per your advice, I have started Super Enzymes, B-12 (2500mg), and vitamin C. And a probiotic. I also take Vitamin D for thyroid, and a multi-vitimim.
Food-wise, I am attempting zero saturated fat, per you recommendations. I am eating small portions, five or six times a day.
Is this a sufficient start?
Rob
Rob the diet is extremely important. What you put in your mouth (after pancreas damage from inflammation) is going to determine whether you heal completely or continue to have problems. And what you put in your mouth means food, drink, medications and well everything. Medications for: high blood pressure and other heart conditions (ACE inhibitors, they are made from snake venom), diabetes, (the list is long), autoimmune disease and anti-rejection (immunosuppressants) and more have all been attributed to causing acute pancreatitis. And as people get older they often find themselves on various prescription drugs that are not safe that increase the risk of pancreas inflammation. My personal 4 workhorse supplements are: 1) Grape seed extract, 2) Curcumin, 3) vitamin C, 4) Pancreatic enzymes. A good multi-vitamin/mineral formula is also necessary for many folks. Info on both (diet and supplements) are on this site
Health Guy
Forget the diet part of my enquiry. I am reading your recommended diet page and can follow that.
Rob
My issues started a few months ago when I noticed an increased heart rate and feeling lethargic after eating large meals. Around that time I also noticed every so often I would have light colored, loose and floating stool.
After going over my friends house several weeks ago I woke up the next day with excruciating constant gnawing pain on the upper right quadrant. I had pizza and beer, maybe 4 total. I had one stool that passed that looked nearly white and o freaked out and went to the ER.
They ran tests and said all my blood work was normal so they weren’t going to do an ultrasound. They referred me to a GI and sent me on my way with some antiacids. I had one other instance where I had an attack severe enough o nearly cried. This was a few days prior to my GI appointment. After that, clear liquid diet, no fat, no alchohol (never averaged more than a beer or two a day) and plenty of water and apple juice. (Read apple juice can help with stone pain)
Reading up on my symptoms I felt for sure it was gallbladder related. I brought this up to the GI and she wasn’t sure. Ordered an ultrasound and the findings for liver, gall bladder and pancreas were clear and no stones, sludge or lesions. I decided to go on the hospital portal and look at my results for myself. A all lover enzymes looked good. Nothing elecates with bilirubin and protease said normal. I looked closer and it said normal range was 9-82 and mine was only at 10. Really close to the bottom.
I searched around on the internet and scared myself seeing that people testing in 5-10 likely had cancer or chronic pancreatitis. With neither looking particuraly good. Obviously, no cancer would be better. I am only 35 which makes it inlokely but not impossible. My GI doc didn’t seem to care and said 0-82 is considered normal. She just had me complete a h pylori breath test today and o wait another 7 days.
I improved with the diet but started dropping a lot of weight. So I tried introducing white meat and olive oil onto onto my diet to stop the free all. Mostly seemed well, untill today, after my test I started to feel unwell.
Here are my symptoms over the last few months: Loose stool that is lighter colored, more recently the color has mostly returned to normal but is like pebbles. The pain is not nearly as severe, but sometimes still dull still on right rib cage. Bloating, especially after meals. Weird stomach sounds. Gas and belching. Fatigue and weakness. Back pain especially mid back up to the shoulder blades. Slight nausea, dizziness, racing heart, feeling hungry but not wanting to eat. A low blood sugar like feeling that makes me jittery. Weight loss, though that may be from hardly eating.
Any thoughts and help would be greatly appreciated. It’s driven my anxiety through the roof, which I have had long standing. I take Lexapro and Klonopin for it. Just thought it was worth mentioning.
Hi Nate – sorry to hear you are not well. You said: “I improved with the diet but started dropping a lot of weight. So I tried introducing white meat and olive oil onto onto my diet to stop the free all. Mostly seemed well, until today, after my test I started to feel unwell.” I’m betting the olive oil was the culprit unless that “white meat” was pork. IF you have gallbladder disease, sphincter of oddi dysfunction, or pancreatitis neither pork nor olive oil will work for most people. Even though you didn’t show stones or sludge the bad news is that it could still be a gallbladder issue simply because if the stones and sludge all passed neither would show on ultrasound. The gallbladder can also develop a “functioning problem” wherein it doesn’t work properly thereby causing pain, nausea, vomiting etc. A HIDA scan can determine whether or not your GB functions properly. Fat causes the gallbladder to become indignant.
Did anyone do blood work and check your lipase and amylase? Both those enzyme raise in acute pancreatitis and sometimes in chronic pancreatitis as well.
Drugs can also cause all kinds of adverse side effects, even death.
Lexapro side effects
Klonopin side effects